EEG Sample: Learning EEG
Greenfield, John, L. et al. Reading EEGs: A Practical Approach. Available from: Wolters Kluwer, (2nd Edition). Wolters Kluwer Health, 2020.
Yamada, Thoru, and Elizabeth Meng. Practical Guide for Clinical Neurophysiologic Testing: EEG. Available from: Wolters Kluwer, (2nd Edition). Wolters Kluwer Health, 2017.
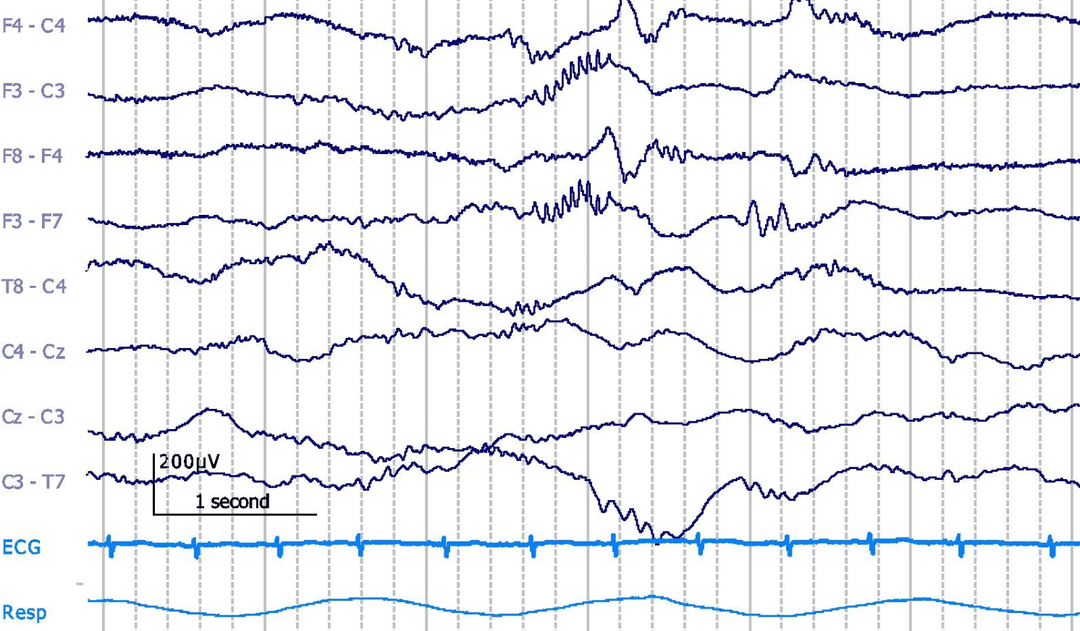
The delta brush has also been called “spindle-like fast,” “brushes,” “rapid bursts,” or “ripple of prematurity.” This pattern consists of a slow wave of 0.5 to 1.5 Hz with an amplitude ranging from 100 to 250μV with a superimposed, rhythmic 8- to 22-Hz activity of 40 to 70μV amplitude. Delta brush appears as early as 27 weeks CA, mainly in the central areas and becomes most abundant at 32 to 34 weeks CA, appearing maximally in occipital and/or temporal, central areas. They are rare at full term and should not be present after 44 weeks CA. They are more common in quiet than in active sleep.
Question:
While delta brush is a normal part of the neonatal EEG, what condition would cause this pattern to be present in the abnormal tracings of an adult patient?
Results
#1. While delta brush is a normal part of the neonatal EEG, what condition would cause this pattern to be present in the abnormal tracings of an adult patient?
ANTI-NMDA RECEPTOR ENCEPHALITIS was first introduced in 2005 and is caused by an autoimmune reaction against NMDA receptors. The patient presents with flu-like symptoms followed by acute psychosis (agitation, paranoia, etc.), altered cognition, and dyskinesia (mouth and lips), and seizures (convulsive or nonconvulsive, or both). Recovery is possible with adequate treatment (steroid, immunoglobulin, and plasmapheresis) but it can be fatal. EEG often shows a unique pattern, referred to “extreme delta brush.” Rhythmic or semirhythmic diffuse or lateralized 1- to 3-Hz delta activity mixed with intermittent 20- to 30-Hz beta or even 30-Hz (gamma) activity superimposed over the delta wave. The pattern usually disappears with spontaneous or induced arousal episodes. Because of extremely fast activity, it is at times difficult to differentiate from muscle artifacts, especially when associated with oral–buccal dyskinesia. Also, the effect of sedative drug (benzodiazepine, etc.) producing beta activity must be ruled out. The rhythmic delta pattern occurs continuously or intermittently, often with sharply contoured waveform, resembling electrographic ictal pattern. In fact, this could be considered status epilepticus (usually nonconvulsive) if the pattern lasts longer than 5 minutes or BRD (brief rhythmic discharges).